Polycystic ovarian syndrome (PCOS) is a hormonal syndrome that effects 8–13% of reproductive-aged women, though it’s estimated that 70% of affected women remain undiagnosed.
It’s considered one of the leading causes of infertility for women, however it’s not just a condition effecting reproductive health. It also raises your risk of developing diabetes, cardiovascular issues, depression, endometrial cancer, pancreatic cancer, and other chronic health and mental health conditions.
While more and more research is being done to better understand the condition, it can be hard to diagnose and even harder to treat.
If you Google “PCOS,” you’ll find a list of different types, but the condition is complex and nuanced — and every individual’s experience with PCOS is wildly different. The “type” doesn’t really matter as much as the hormonal imbalances that exist within your body and the symptoms you’re experiencing.
To be medically diagnosed with PCOS, you must present with two of the following factors:
Have biochemical or clinical signs of hyperandrogenism
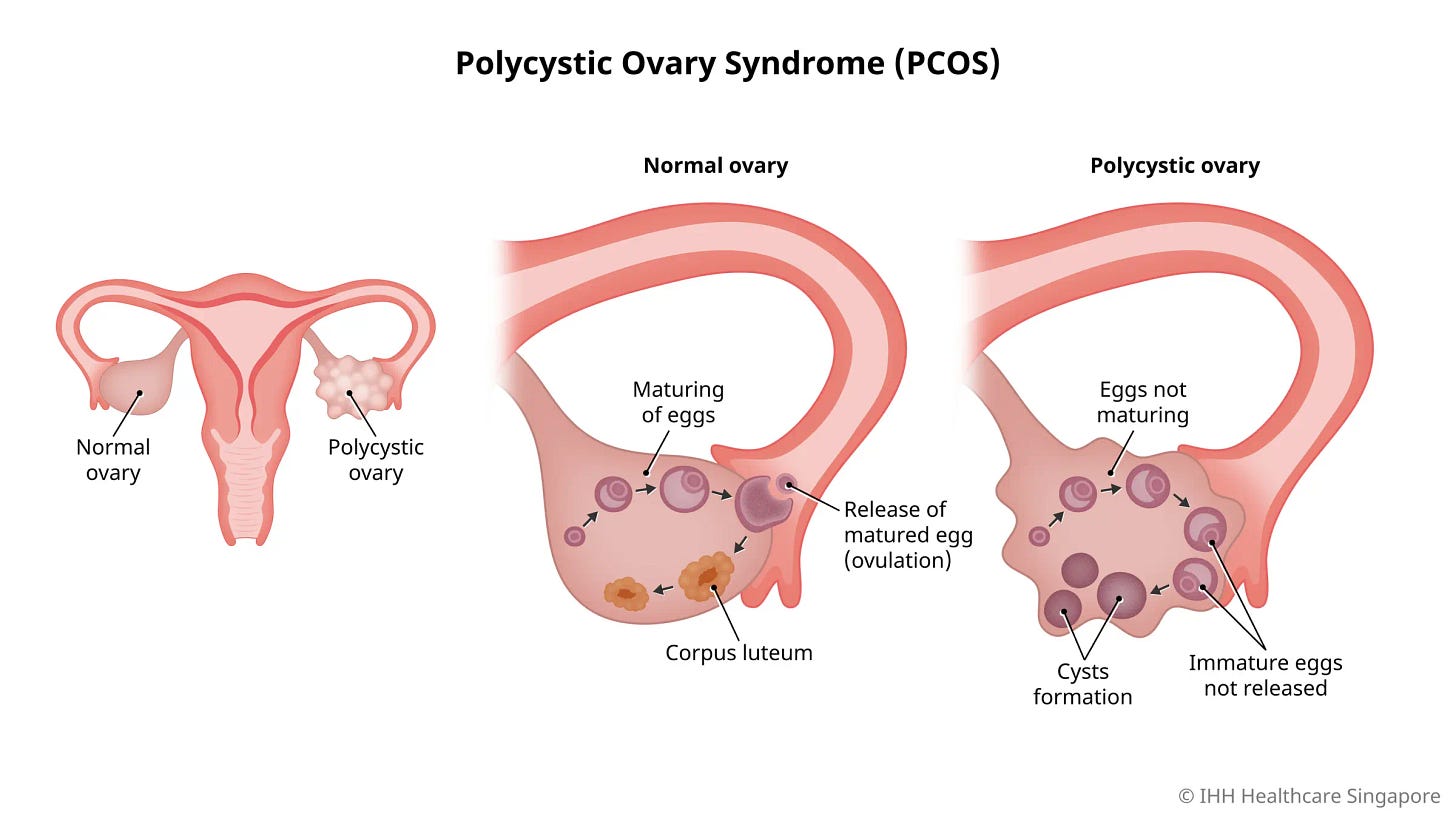
Have polycystic ovaries (as shown in the graphic below)
Have an irregular menstrual cycle
The path to diagnosis can be challenging, sometimes taking two or more years, as many don’t realize that their symptoms are associated with this condition.
You may have excess hair growth on your face or arms, for example, not knowing this is a result of excess hormones. You may be struggling to conceive, not knowing that your 45-day menstrual cycle is considered irregular.
While some can be diagnosed with a simple physical examination, many require an ultrasound and/or blood tests to confirm the PCOS diagnosis.
After getting a diagnosis, the path to treatment can be especially changing.
First, you have to figure out what specific issues your dealing with and how best to treat them, which is no easy feat.
In addition to having high androgen levels and/or multiple cysts on your ovaries, do you have insulin resistance? Are you experiencing metabolic health issues? Do you have inflammation? Are you battling hirsutism? Do you have insomnia? Or sleep apnea? Or anxiety? What about depression?
All of these symptoms and/or conditions can be associated with PCOS, even if they aren’t directly tied to the diagnosis itself. This is one of the many reasons why medical experts believe the diagnostic criteria is outdated and should be reassessed.
While there are many different treatment options available, there’s no single cure for the condition. Often, people find that a combination of the following works best to address their various symptoms:
Lifestyle changes (ex. exercise, diet, behavioral intervention)
Supplementation (ex. vitamin D, inositol, CoQ10)
Medication (ex. Metformin, spironolactone, clomiphene, letrozole)
Surgery (ex. laparoscopic ovarian drilling, transvaginal hydrolaparoscopy)
Figuring out the right tailored treatment plan for your specific needs can take years and years and may require you to visit a number of different professionals, such as an ObGyn, an endocrinologist, a nutritionist, a dermatologist, a therapist, etc.
It’s not as simple as taking an oral contraception or losing weight — and if this is what your doctor recommends for treatment, please find another doctor. In order to properly manage the condition and reduce your risk for other conditions, you really need to address the underlying issues.
This process can be strenuous and emotional, especially if you don’t have an advocate or support team guiding you through.
Okay, okay, you’re wondering, but what about that social media influencer who managed to lose weight, eliminate excess hair growth, regulate her cycle, and get pregnant, all without medication or surgery? Surely she knows what works!
Maybe… but just because it worked for her doesn’t mean it will work for you. Remember, everyone’s experience of PCOS is unique, so every treatment plan should be individualized — and the only way to know if something is really working is to keep testing.
If it sounds exhausting, that’s because it is.
Thankfully, PCOS is getting more attention than ever before and with that comes more research, greater understanding of the condition, and better, more accessible treatment options. We now know, for example, that PCOS is a lifelong condition and not something that just effects women of child-bearing age. We also know that the majority of people with PCOS experience insulin resistance — and this raises a person’s risk of developing other health conditions like type 2 diabetes and heart disease.
What’s exciting is that more and more companies are erupting in the space (like Allara Health, Pollie, Modern Fertility, and Almond ObGyn) and tackling the condition with a multidisciplinary and in some cases virtual approach. This can be especially beneficial for those who have faced discrimination or gaslighting in the traditional healthcare space, and want to connect with a provider who has a strong background in working with PCOS patients.
All this is to say, don’t lose hope. Just because you’ve been suffering with PCOS symptoms for years doesn’t mean you’ll always suffer with them. Chances are you just haven’t found the right treatment yet…
Q&A with Christy Evans, MD, Co-founder of NewDAWNAfrica and The Village for Mamas, as well as the Board Certified ObGyn and Head Physician at Almond ObGyn.
Dr. Evans is a functionally trained physician who takes a root-cause approach to healthcare. In her day-to-day work with Almond ObGyn, a tech-enabled, modern ObGyn in Los Angeles, Dr. Evans works with patients to understand their comprehensive history in order to provide holistic and highly personalized care.
Q: What does a root-cause approach entail?
Traditional medicine often focuses on urgent matters and utilizes surgery and medications, which is really important, but a lot of the things that women suffer from are chronic conditions and in this aspect, I think the traditional medicine approach has failed us.
What I like about a functional, root-cause approach is that it forces us to take a look at our patients, individually, on a personal level, and focus on the main pillars of health (sleep, nutrition, movement, stressors). That’s where it starts. Then we can build a more holistic picture of what’s going on for the patient and better understand the root cause of why that patient might not be feeling well and really optimize her health.
With this approach, I feel like I’m able to provide much better care and build a much more comprehensive plan for them.
Q: What does this look like in practice?
Oftentimes in traditional visits, providers just don't have the time. Someone comes in and they say they are having all these complex issues that may be related to their hormones and they think they have PCOS, but the provider only has five to 10 minutes with them, which isn’t enough and is frustrating. It’s important to truly get to know them in a really comprehensive way before diving into those things. This is one of the reasons why traditional medicine fails.
At Almond, I go through a comprehensive history on the first visit, simply talking with them, getting to know them, their medical history, what their health goals are, and what their health concerns are. Having that foundation of learning about the person, we can then create a care plan that can address each of those things in a more comprehensive way.
Q: Why is PCOS so hard to diagnose?
I think it’s both easy and hard. PCOS is a syndrome which means it is a combination of different presentations and symptoms. It is experienced differently by different people. The most commonly used criteria is the Rotterdam criteria that's used by a lot of the professional societies. Women need to have two of the three categories to be diagnosed with PCOS. Not every woman is going to have polycystic ovaries. Not every woman is going to have characteristics of elevated testosterone, and not every woman is going to have oligomenorrhea, though that is often the number one thing that we see with PCOS.
When a patient presents with irregular or skipped cycles and symptoms of elevated testosterone, it can seem very straightforward. When it's a little bit more ambiguous about what's going on, maybe they have irregular cycles, we have to do some lab work, and it might take more investigation. Regardless, I usually do recommend more comprehensive lab work, because PCOS can be associated with so many other conditions, metabolic conditions, increased risk of diabetes, cardiovascular disease, and hyperlipidemia. I look more comprehensively at what their overall health picture is when I'm concerned about PCOS.
Q: Can you talk about the different types of PCOS?
There are some providers that will describe PCOS in four different ways. I approach PCOS with the goal of understanding the underlying hormone imbalance. Fundamentally it is a metabolic disorder. Upwards of 70% of women who have PCOS have some level of insulin resistance. When a patient has insulin resistance, it can lead to increased insulin in circulation, which can lead to increased testosterone, and increased numbers of cysts, which can then result in a lack of ovulation or less ovulation, hence the abnormal cycles and symptoms like acne and facial hair.
Q: What about post-pill PCOS? Does that mean being on the pill caused PCOS?
That’s a common misconception. A lot of women are put on birth control pills for a number of different reasons, maybe to regulate their cycles, as a teenager. While I have no doubt that there are many times when women actually do have PCOS as a teenager, the problem is that our hormone systems are pretty immature when we're teens and into our early 20s.
While you’re on the birth control pill, we don’t actually really know what's going on with your cycles. We don't know whether you would have had balanced hormones to be ovulating regularly, so it’s not until you get off the birth control pill and actually learn what your cycles are like for the first time in many years or decades that you’re able to uncover Issues with your cycle. It’s not that the pill causes these new symptoms, but rather that it did such a good job of masking the symptoms that whole time. This is actually one of my favorite times to be working with patients, because I get to learn with them and we get to figure out what’s going on with their cycle, what symptoms they’re experiencing, and track their ovulation, whether it’s for the goal of getting pregnant or for optimizing their health. That information can be really valuable for evaluating a woman’s overall health.
Q: When treating PCOS, why is it important to combine medical treatment with lifestyle changes as part of the intervention?
There are so many reasons why a woman with PCOS will come to us for help. Oftentimes they're concerned because they want to get pregnant, but they're not ovulating or it's difficult to track their ovulation. Some women come to me because they're annoyed by some of the symptoms like acne or weight gain, and some are not necessarily interested in fertility, but want to feel better and optimize their health.
When a woman has a diagnosis of PCOS, we need to understand her main health goals then develop a plan for how we can achieve them. To me, it always comes back to ovulation. If a woman is ovulating regularly, it tells me so much about her overall health, because it requires the brain and the ovaries and the uterus to be in communication with each other in a really beautiful, integrated way.
I may be biased, but I think the menstrual period is a fundamental vital sign. It’s the one thing I ask about right away and that I spend a lot of time talking about. In terms of treating PCOS, we focus on optimizing her hormonal and metabolic health to achieve more regular ovulation. This means tracking ovulation and addressing the pillars of health – sleep, nutrition, exercise and exercise in the right way, meaning not too much, not too little, and managing stressors in your life. Sleep is number one. It’s so crucial. A lot of people really struggle with their sleep. If you have a poor quality and poor quantity of sleep it can impact all the other pillars of health.
As a provider, I’m so excited I get to talk about all of these things and dive into this with my patients in a comprehensive and intensive way. The PCOS program at Almond also allows patients to work one-on-one with a health coach, who can implement the things we’re working on. If we want to improve nutrition, we can consider what tools are needed on a daily basis to regulate blood sugars and put the right nutrient-dense foods into our bodies. The same things with exercise, sleep, and life stressors.
Q: Why is PCOS treatment so complex?
There’s no one simple pill. Oftentimes women are prescribed birth control, which can be an excellent solution for regulating wildly irregular cycles. It can add a level of predictability. When women are not having their cycles, there's estrogen in the body that’s not countered by progesterone, and that can be dangerous for the lining of the uterus, so having a birth control in place protects the lining of the uterus, called the endometrium, from endometrial polyps and cancer, so it can be an excellent tool for women who have PCOS. But let me be clear, birth control pills are not a treatment. It might help manage symptoms, but it takes a lot of work from the provider and the patient to fine tune their lifestyle to really address the underlying issues, long-term health, and support healthy living.
Q: Can you talk about Almond’s new PCOS program?
Being able to do this is a dream for me. Our PCOS program is an intensive 4 month, structured program that pairs our patients with clinicians and health coaches to dive into their underlying issues and work toward their health goals. It’s comprehensive - patients get hour-long visits, with robust lab work and evaluations, tons of education, and detailed, personalized care plans involving concrete and actionable lifestyle changes. What does this look like? In my opinion, sleep is fundamental, especially for regulating our blood sugar levels. That’s one of the first things I focus on. Another is gut health. For some, this might mean trying an elimination diet or cutting out certain inflammatory foods, or using a probiotic. Each patient needs a personalized plan. Exercise is also important. We want our patients moving their bodies. Ultimately, this comprehensive approach will serve our patients well.
The whole team is amazing. Everyone's really compassionate and motivated to get patients feeling better, and not just treating the symptoms, but figuring out the root cause.
Q: Are you expecting more patients looking for a PCOS diagnosis or those with PCOS looking to get treated?
I expect both scenarios. Nearly every day I have women coming to me saying they think they have PCOS because of what they hear on social media. I have others, too, who have all the symptoms of PCOS but have never heard of it. There’s a lot of misinformation out there and at the same time a lot of women are under informed. With growing metabolic dysfunction in this country, we are seeing more and more women suffering from PCOS. Additionally, there is not nearly enough research being done to truly understand PCOS.
Q: What’s the one healthy habit you can’t live without?
Getting great quality sleep. This means having great sleep hygiene, prioritizing unwinding at the end of the day, and perhaps most indulgently, getting sunlight first thing in the morning to regulate my circadian rhythm. I go out to my garden, still in my pajamas, before brushing my teeth, and get direct sunlight. It just feels good to be in nature and see the trees and flowers and start my day that way.
Mind
There’s a new FDA-approved medication treatment for schizophrenia, which could be life-changing for those with a treatment-resistant case.
Body
You know you’re getting older when your generation is starting menopause.
New study shows that more than half of women diagnosed with fibroids are offered hysterectomies compared to minimally invasive procedures and 17% wrongly think hysterectomies are the only treatment option.
Hormone therapy (often used during menopause) may have positive overall outcomes for cardiovascular health, according to a new study.
Beyond
What’s the best city for women’s economic & social well-being + health care & safety? Columbia, Maryland… followed by Fremont, CA and Huntington Beach, CA. The worst? Jackson, Mississippi. See where your city ranks.
Just last week, the first lady announced a $500 million investment into women’s health research.
Want to learn about other women’s health and mental health topics? Consider subscribing to Steeped in Wellness or share with a friend.